When Milk No Longer Works For You, Here Is What You Need To Know
When people are lactose intolerant, they are not able to tolerate the lactose in cow’s milk because it can be difficult for people to digest, resulting in side effects such as nausea, gas, cramps, bloating and diarrhea. Many adults develop lactose intolerance in later life, and this intolerance typically worsens over time and leads to progressively worse symptoms.
In the case of a milk allergy, this is completely different from lactose intolerance and can cause potentially strong and dangerous reactions such as anaphylaxis and vomiting. One notable difference is that milk allergies elicit an immune response. Milk is the third most common food (after peanuts and tree nuts) to cause anaphylaxis. In individuals with milk allergies, their immune systems trigger the production of immunoglobulin (IgE) antibodies to neutralize the protein (i.e., casein and whey) in milk. The next time that the body of someone with a milk allergy comes in contact with these milk proteins, the antibodies recognize them and signal the body to release histamine and other chemicals which cause a wide range of symptoms.
Cow’s milk is a good source of calcium, potassium and high quality protein all of which are important for bone health, blood pressure regulation and muscle growth and development. Additionally it’s a great source of vitamin A, magnesium, zinc and thiamine.
Cow’s milk is often a staple beverage on many tables in the U.S. As we move around the world, rates of dairy consumption vary as does lactose intolerance. In the U.S, although milk is a staple beverage, data tells us that lactose intolerance impacts 95% of Asian Americans, 74% of Indigenous Americans, 70% of Black Americans, 53% of Mexican Americans and 15% of Caucasians. Globally, most of the world’s largest milk consumers are located in Europe and the prevalence of lactose intolerance is low in many European countries, specifically Central and Northern Europe.
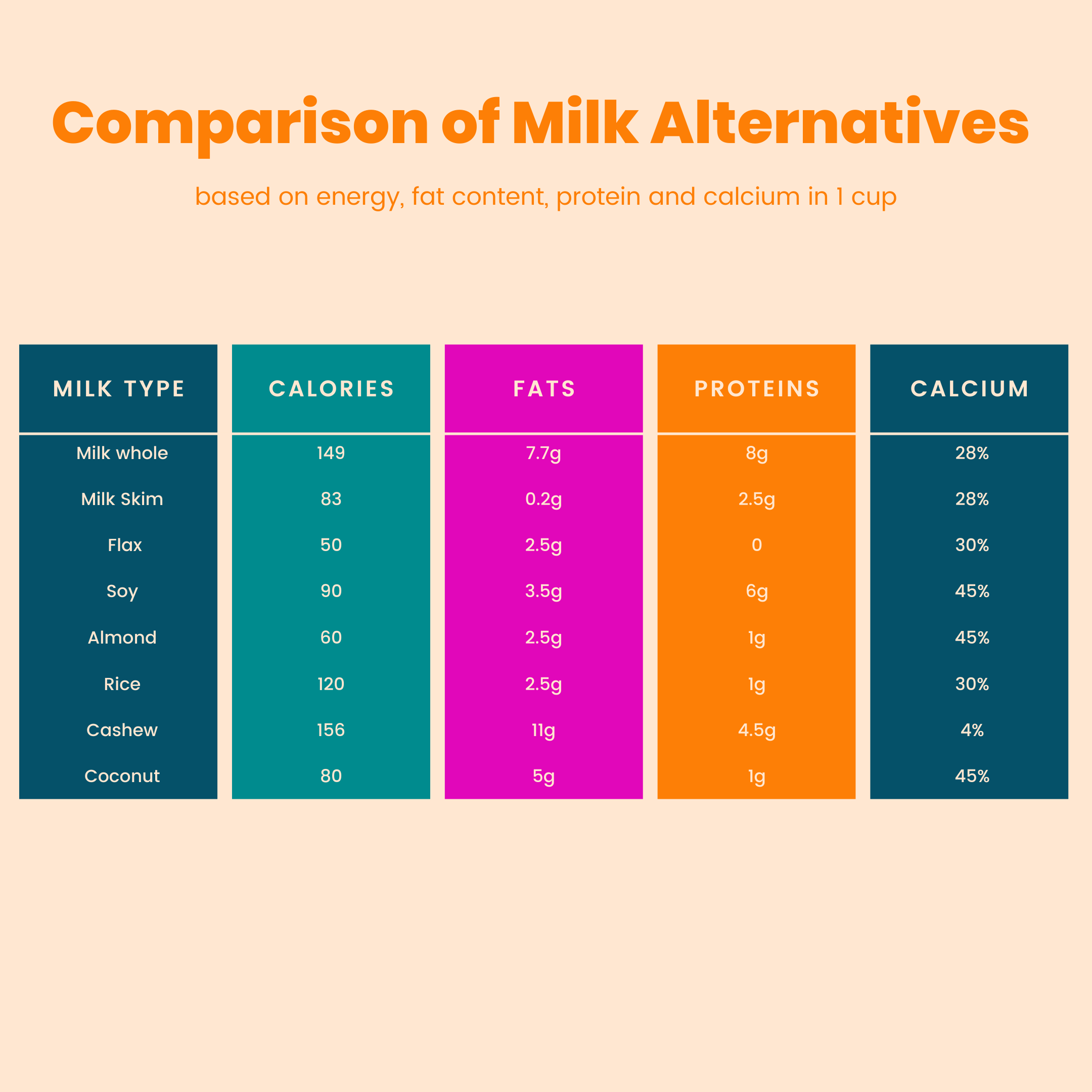
Once milk is removed from the pattern of eating, the key is to find a replacement that provides the desired mouthfeel and nutrient profile.
Table 1 is a comparison of alternatives to cow’s milk based on energy, fat content, protein and calcium in 1 cup
Almond, coconut, and cashew and oat milks provide less than half of the protein provided by soy and cow’s milk. Soy milk, almond milk, and oat milk contain at least half the fat of cow’s milk. Almond milk contained the most calcium of the milks surveyed. Quantities of folate and vitamin B12 were most notably decreased in almond milk, while soy milk had almost double the amount of folate and vitamin B12 present in cow’s milk.
The top food allergens in the U.S are wheat, eggs, peanuts, fish, crustaceans, tree nuts, and soybeans. Together they account for more than 90% of all IgE-mediated food allergies.
Among the non-dairy alternatives, almond-based substitute was the most allergenic with the highest IgE reactivity, while the coconut milk substitute was lowest. For IgG and IgA immune-reactivity, soy was first, with coconut again the lowest.
Table 2 is a comparison of milk alternatives based on texture / mouthfeel and allergens to be aware of.
With all of the options available, it’s important to be an informed consumer and make a choice that meets your personal preferences as well as nutrition needs.
References :
- United States Department of Agriculture’s Food Data Central database. https://fdc.nal.usda.gov/
- https://pubmed.ncbi.nlm.nih.gov/30156521/


Leave a Reply