Type 2 Diabetes Mellitus: Symptoms, Causes, and Treatment Options
It’s National Diabetes Month, which means this is the perfect time to take a deep dive into the fastest growing global epidemic of our time: type 2 diabetes.
While we’re all familiar with this chronic disease and likely have either been diagnosed with it ourselves or know someone close to us with this diagnosis, it’s important to remain educated on a few elements: what it actually is along with the top signs, causes, and risk factors as well as the outlook if you’re diagnosed with it.
Join me as I take a closer look at each of these areas and discuss what you can do if you’ve been recently diagnosed.
What is Diabetes?
So, what exactly is diabetes?
First, there are two different types of diabetes mellitus (more commonly known simply as diabetes): type 1 and type 2.
Type 1 diabetes occurs when the body creates little to no insulin due to the destruction of the insulin-producing pancreatic beta cells due to an autoimmune reaction.
It is an autoimmune disease most often diagnosed during childhood and sometimes referred to as juvenile diabetes. [1]
Conversely, type 2 diabetes is multifactorial, where the body secretes appropriate amounts of insulin resulting in excess blood sugars remaining in the bloodstream and or excess insulin that is not utilized (insulin resistance). [2]
Think of insulin as the carrier that moves excess sugar out of circulation and into the cells for use. When this mechanism goes awry, the outcome is unstable blood sugars.
While genetics and factors outside of our control can play a role in the development of type 2 diabetes (see the following section on risk factors for more information), there is only one real cause: the body not utilizing insulin properly.
Let’s take a closer look at each of the risk factors and how they can contribute to insulin resistance and the development of type 2 diabetes.
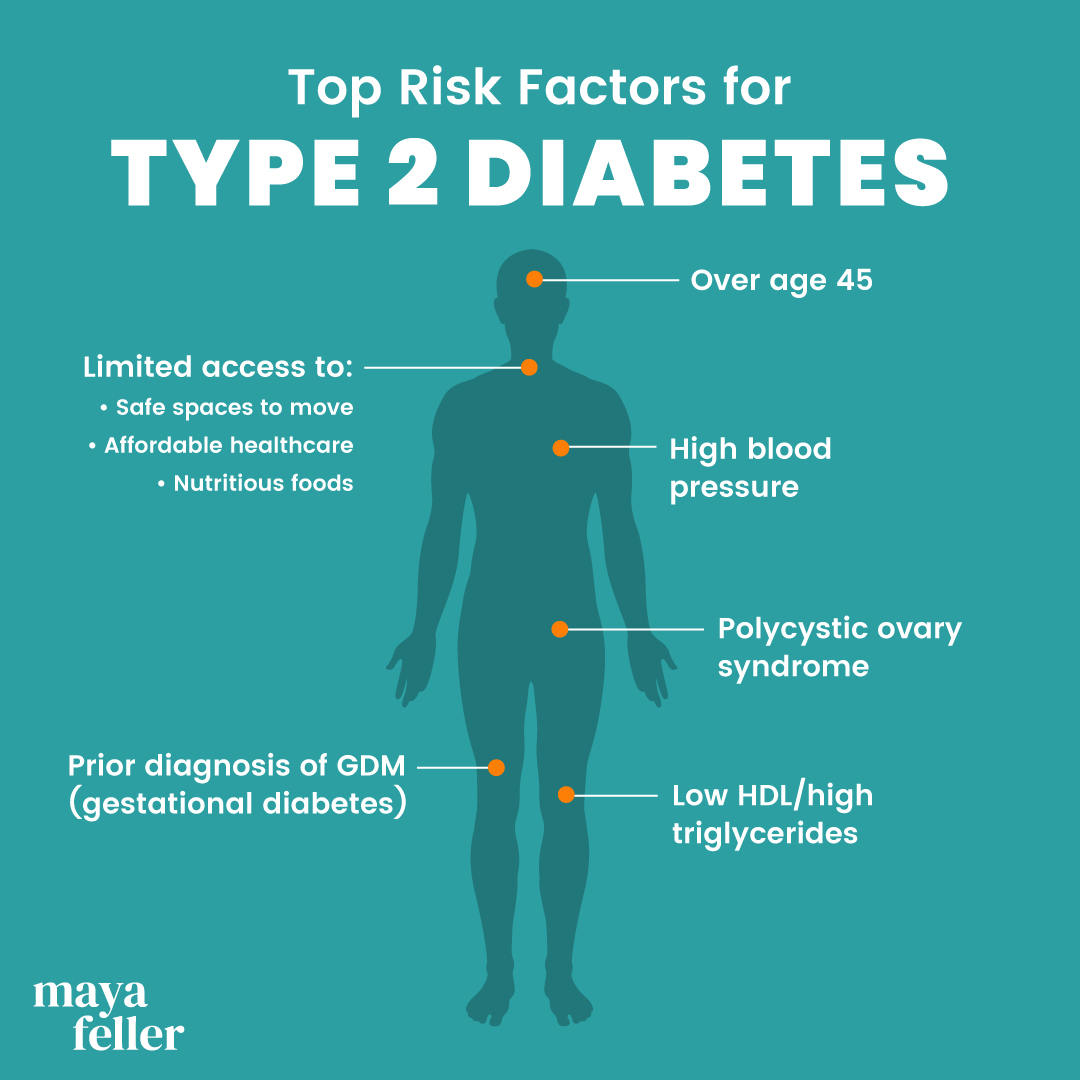
Risk Factors for Type 2 Diabetes
Here are a few of the top risk factors for type 2 diabetes.
1. SDOH (Social Determinants of Health)
Research has shown that regular exercise, eating nutritious foods, and access to healthcare can decrease your risk of developing type 2 diabetes. [3, 4]
In fact, research has shown that adults with limited income , restricted or toxic environmental housing, lack of access to nutritious foods, limited access to affordable and quality healthcare, and a lack of social support are more likely to be diagnosed with type 2 diabetes.
Specifically, people who have “middle income” are 40 percent more likely to develop type 2 diabetes than those with “high income.” That number jumps to 74.1 percent for those who are classified as “near poor” and 100.4 percent for those classified as “poor.” [5]
In the U.S., racial and ethnic minorities are disproportionately impacted by type 2 diabetes and more likely to not have access to the services that are needed to achieve optimal health.
2. Over age 45
According to the CDC’s 2020 National Diabetes Statistics Report, when you’re age 45 or older, your risk of developing type 2 diabetes almost quadruples in comparison to when you were 44 or younger. [6]
Researchers have surmised that this increase in risk is due to the fact that older adults are more likely to experience increasing insulin resistance along with age-induced impairment of pancreatic islet function. [7] (These islets are cells within the pancreas that produce and release hormones that regulate your blood sugar levels.)
As we age, all systems within our body as well as immune function decrease in terms of efficacy.
3. Polycystic ovary syndrome (PCOS)
It’s been well established for several years that there’s a link between being diagnosed with PCOS and an increased risk of developing type 2 diabetes. But just how strong is that link?
According to a 2017 study, women with aa PCOS diagnosis were four times more likely to develop type 2 diabetes than women without the diagnosis. Additionally, they were diagnosed, on average, four years earlier (at age 31) than women without PCOS (at age 35). [8]
The reason? The researchers noted that prior studies have shown that insulin resistance is part of the pathogenesis of PCOS.
4. Prior diagnosis of GDM (gestational diabetes)
It’s long been documented that women with a history of GDM are at greater risk of developing type 2 diabetes. But you may be surprised to hear by how much.
According to a 2020 meta-analysis reviewing studies including over 1.3 million women, those with a history of GDM were nearly 10 times more likely to develop type 2 diabetes than those without GDM. [9]
Interestingly the risk is highest in the first five years after a GDM diagnosis and increases at a slower rate after 10 years post-birth.
5. Low HDL/high triglycerides
Another effect of insulin resistance is that it often results in high triglycerides and low HDL numbers—so much so that low HDL numbers are now considered a risk factor for developing type 2 diabetes. [10]
Interestingly, because HDL is known to help to stimulate insulin secretion, researchers have surmised that having low HDL may actually contribute to blood sugar instability. [11]
6. High blood pressure
Researchers have known for quite some time that diabetes and high blood pressure are linked. In fact, those with high blood pressure are more likely to be diagnosed with type 2 diabetes and vice versa.
The endocrine system functions as a whole, so when one system goes out of balance (homeostasis), there is an increased risk for a comorbidity to develop.
According to a 2015 meta-analysis on 4.1 million people, people with 20 mm Hg higher systolic blood pressure readings were 58 percent more likely to develop type 2 diabetes. [12]
Signs of Type 2 Diabetes
Now that you know a bit more about the risk factors, let’s take a look at some o the top signs of type 2 diabetes: [13]
- Extreme thirst
- Frequent urination
- Tiredness and listlessness
- Nausea
- Dizziness
Treatment Options for Type 2 Diabetes
One common question for those who are diagnosed with this disease is: Can type 2 diabetes be cured?
Currently, there is no known cure, and some people do go into remission, type 2 diabetes can be managed by following an individualized balanced pattern of eating, making time for intentional movement, and being connected to medical care. [14]
I recommend cultivating a healthcare team that will meet all of your needs, which may include a primary physician and endocrinologist, as well as working with a Registered Dietitian to develop a plan tailored to your unique situation and needs.
When it comes to nutrition, individualization and balance are the key. Learning where and when to make food swaps, increasing your carbohydrate literacy, and keeping your cultural foods at the table are all keys to success—all of which I cover in my book, The Southern Comfort Food Diabetes Cookbook.
The great news is that there are plenty of ways you can still enjoy your favorite sweet treats; they just require some simple swaps, like what I did with these fried apples! With the right approach, you don’t have to feel like you’re sacrificing
How to prevent type 2 diabetes
There are some steps you can take to reduce your risk of developing type 2 diabetes, and they include:
- Making time for intentional movement.
- Cultivating a balanced and nutrient-rich pattern of eating.
- Engaging in stress-reducing activities.
- Listening to your body and getting regular check-ups.
Remember, you have the power to take back your health and make a difference in your daily life.


Leave a Reply